New in Neuroscience: How do different mutations in the same gene contribute to different neurological disorders?
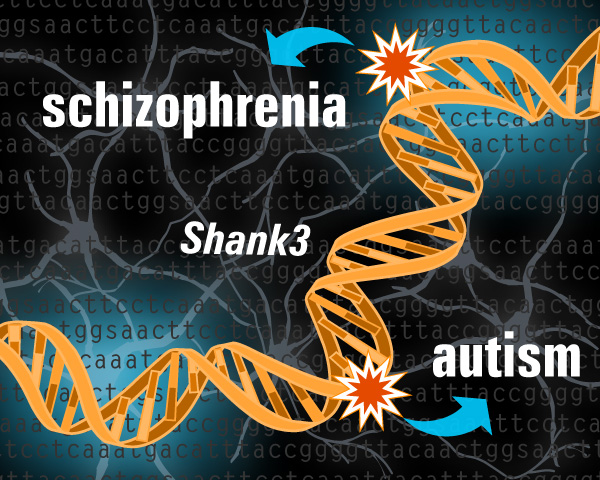
/Each year, approximately 61.5 million Americans are afflicted by a mental illness. Although we have not yet determined the underlying cause of these disorders, scientists believe that genetic mutations play a major role. Human genetic testing has identified multiple “risk genes” that are associated with major psychiatric disorders, but little is known about how mutations in the same risk gene can contribute to different disorders. For example, autism spectrum disorder (ASD) and schizophrenia share common features such as interpersonal and cognitive deficits, but they are currently defined as two different disorders with largely unknown etiologies. However, recent genetic studies have revealed that both disorders maybe caused in part by different mutations in a group of genes linked to synaptic transmission (neurotransmission).
Synapses are the sites of communication between neurons. Each synapse consists of a presynaptic ending that contains neurotransmitters (signaling molecules) and a postsynaptic ending with receptor sites for the neurotransmitters to bind to and activate. Shank proteins, consisting of Shank1, 2 and 3, function as master organizers of the postsynaptic endings since they can recruit and form complexes with receptors, signaling molecules, and other proteins. Previous research has shown that one kind of mutation in Shank3 is found in some people with ASD, whereas a different kind of mutation in Shank3 is found in some people with schizophrenia. In a paper recently published in the journal Neuron, Yang Zhou and colleagues at MIT use mice to understand how different mutations in Shank3 can result in these distinctive disorders.
Using two mutant mouse lines, the authors demonstrate that the Shank3 mutations found in patients with ASD and schizophrenia have shared and distinct phenotypes at the behavioral, synaptic, and molecular levels. Behaviorally, juvenile mice with the ASD-linked mutation showed impaired social interactions such as showing no preference to interact with other mice over inanimate objects. These symptoms found in young mice coincided with the early onset of ASD symptoms in people. Adult mice with the schizophrenia-linked mutation showed behavioral symptoms of social dominance, coinciding with some of the negative symptoms seen in people with schizophrenia who oftentimes exhibit symptoms of social withdrawal and anxiety.
Interestingly, the authors found that the ASD-associated mutations caused synaptic transmission defects in the striatum, a subcortical part of the forebrain and a critical component of the reward system. The striatum has been implicated in the pathophysiology of autism: using resting state functional magnetic resonance imaging, researchers have previously found that compared to normally developing children, children with ASD have abnormal circuits in the striatum. The authors of this study also found that the schizophrenia-associated mutations caused profound synaptic defects in the prefrontal cortex of the brain, which is responsible for planning complex cognitive behavior and decision-making, as well as moderating social behavior. Dysfunction of the prefrontal cortex has been closely linked to patients with schizophrenia. In fact, abnormalities in this brain region can be found even before patients begin to exhibit clinical symptoms.
The central dogma of molecular biology—which explains how genetic information flows within a biological system—states that DNA makes RNA, which makes proteins. At the molecular level, the authors found differential stability and regulation of Shank1, Shank2 and Shank3 mRNA. Although both Shank3 mutations resulted in premature stop signals in the mRNA, truncated Shank3 proteins were only found in mice with the schizophrenia-associated mutation and not the ASD-associated mutation. Using a technique called quantitative real-time PCR, which allows a scientist to measure the amount of mRNA in a cell or tissue, the authors consistently observed dramatically reduced levels of Shank3 mRNA in mice with the ASD-associated mutation. Although Shank3 mRNA levels from the schizophrenia-associated mutants were significantly lower than those from normal littermate controls, they remained significantly higher than those from ASD-associated mutants.
These data suggest that Shank3 mRNA with the schizophrenia-associated mutation are more stable than Shank3 mRNA with the ASD-associated mutation, thus resulting in translated Shank3 proteins in schizophrenia-associated mutants and not ASD-associated mutants. Interestingly, the amount of Shank1 and Shank2 mRNAs were significantly increased in the ASD-associated mutants but not the schizophrenia-associated mutants, suggesting that increases in the amount of Shank1 and Shank2 may act to partially compensate for the loss of Shank3 protein in the ASD-associated mutant mice. If the mRNA with the ASD-associated mutation are in fact less stable than mRNA with the schizophrenia-associated mutation, this could perhaps explain why behavioral symptoms of ASD emerge earlier than those of schizophrenia in both mouse models and human patients. In fact, ASD can be detected in children as early as 18 months of age or younger, whereas the typical age at diagnosis for schizophrenia is around 18-25 years of age.
Despite strong evidence from clinical and genetic studies, little has previously been known about how different mutations in the same gene can contribute to different psychiatric disorders. Using two new mouse models with Shank3 mutations commonly found in ASD and schizophrenic patients, the authors found distinct and shared defects at behavioral, synaptic, and molecular levels. Although the study provides strong evidence in its characterization of similarities and differences between the two mice models, it does not provide sufficient causality into how the specific mutations result in mutation-specific defects and behavioral abnormalities. In addition, the authors make multiple claims regarding juvenile and adult ages but only provide one time point for each age category. In order to substantiate those claims, a more-detailed time course is required. Future studies should further analyze these two novel mutant mouse lines in order to gain a more precise understanding of synaptic development and function.